Help us improve our information
We need your help to improve our information to better support people with Crohn’s and Colitis. Fill in our short survey to let us know what we're doing well and how we can better meet your needs.
Last reviewed: April 2024
Next review date: April 2027
If you have Crohn’s or Colitis, you may develop a fistula. A fistula is a tunnel that connects one organ to another part of your body. Fistulas can cause unpleasant symptoms. But there are different treatments and ways to manage them.
This information is for people affected by Crohn’s or Ulcerative Colitis. Fistulas are not associated with Microscopic Colitis.
This information will help you to:

We need your help to improve our information to better support people with Crohn’s and Colitis. Fill in our short survey to let us know what we're doing well and how we can better meet your needs.
Although being diagnosed with a fistula is quite difficult and scary at the beginning, once you get used to it, it does get easier to deal with. You just get on with your life as normal and do most of the things you did before.
Claire, age 38
Living with Ulcerative Colitis
A fistula is when a tunnel develops that connects one organ to another part of your body. These tunnels can connect one internal organ to another or to the skin. A fistula can develop in any part of the body, but many involve the gut. A fistula is different to a fissure. A fissure is a small tear in the skin, often around the bottom.
Around 1 in 3 people with Crohn’s develop a fistula at some point in their life. This risk is lower in Ulcerative Colitis. Some people develop a fistula before they are diagnosed with Crohn’s or Ulcerative Colitis.
Perianal or anal fistulas are more common in men than women. It’s not clear if people from some ethnic groups are more likely to develop fistulas than others. For example, some studies have found that anal or perianal fistulas might be more common in Afro-Caribbean, South Asian or Korean people. Others have found that Chinese people may have lower rates of fistula development. More research is needed to know if and why some ethnic groups are more likely to develop fistulas.
Children can also develop fistulas. You might be more likely to develop an anal or perianal fistula if your Crohn’s or Colitis started when you were a child. Our Supporting your child information has more advice for parents of children with Crohn’s or Colitis.
Experts do not fully understand what causes fistulas. Certain genes and gut bacteria may play a role. If you have Crohn’s, the cells involved in healing may not work as they should. It is not your fault if a fistula develops.
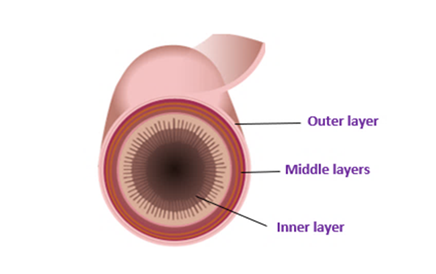
Bowel layers
Fistulas are more common if you have Crohn’s. This is because inflammation can spread through all the layers in the bowel wall. This inflammation can cause small leaks and abscesses to form. An abscess is a buildup of pus. As the abscess develops it may hollow out a chamber or hole. This can become a channel linking the bowel to:
The longer you have Crohn’s, the more likely you are to develop a fistula. Fistulas can happen anywhere in the gut, but commonly occur above strictures. Strictures are narrowed areas of the gut. Increased pressure and inflammation above strictures may cause fistulas to develop.
In Ulcerative Colitis inflammation does not affect all layers of the bowel wall. This means fistulas are less likely to form. Fistulas are not associated with Microscopic Colitis.
Fistulas associated with Crohn’s:
Fistulas associated with Ulcerative Colitis:
Health professionals may use some of these words to describe where a fistula is.
|
Word |
Meaning |
Fistula type |
|
|
|
|
|
Peri |
around |
Perianal - around the bottom (anus) |
|
Entero |
bowel or gut |
Enteroenteric – linking sections of the gut |
|
Vesical |
bladder |
Enterovesical – links to the bladder |
|
Cutaneous |
skin |
Enterocutaneous – opens onto the skin |
|
Colo |
colon – part of the large bowel |
Enterocolonic – links the colon to another part of the gut |
|
Recto |
rectum – part of the large bowel |
Rectovaginal – links the rectum to the vagina |
|
Inter |
between |
Intersphincteric – between two sphincters |
There are different types of anal fistulas. Understanding the muscles around the bottom (anus) may help you understand the different types. Doughnut shaped muscles, called the anal sphincters, surround the anal canal. The anal canal is the final bit of bowel where poo travels before leaving the body. The anal sphincters allow you to control when you open your bowels to poo.
There are two anal sphincters:
Damage to these muscles can mean you have less control over farting and pooing.
The anal sphincters
This diagram shows the position of the muscles around the anal canal where poo travels. As well as the anal sphincters, there are the pelvic floor muscles. These also help you to release pee, poo and fart, or to delay releasing until you reach a toilet.
The name of a fistula tells you where they are and if they involve the external or internal sphincters.
The symptoms you have will depend on where your fistula is.
Anal fistula. The first sign can be a tender lump in the area around the bottom (anus). This is often followed by pain and irritation which gets worse when you sit down, move around, poo or cough. Pus, poo, or blood can drain from the fistula opening
Bladder fistula. Symptoms include passing air, pus, or poo when you pee. Some people find pee may leak from the bottom. You may also have an urge to pee very often and get urinary tract infections (UTIs). You may need to take antibiotics to treat a UTI.
Vaginal fistula. Symptoms include pain which may be mild to severe, depending on how big the fistula is and where it is. It may make having vaginal sex painful, or even impossible at times. Some people with vaginas find they fart, pass poo, or pass pus through the vaginal opening.
Bowel to skin fistula. Symptoms include leakage of gut contents through the skin. This can lead to diarrhoea (loose or liquid poo) and dehydration (when your body loses more fluids than you take in). It may also cause malnutrition (a serious condition that happens when your diet doesn’t contain the right amount of nutrients) and upset the body’s chemical balance.
Bowel to bowel fistula. Symptoms depend on how much of the bowel is affected and the location of the two ends of the fistula. Where only a short section of gut is skipped by the fistula, people may not have any symptoms. When a large part is involved, people can experience diarrhoea, dehydration and malnutrition.
The tests you will need depend on the type of fistula you have. Your IBD team will aim to find out:
Anal fistula
If your doctor suspects an anal fistula they will carry out a physical examination of the skin around the bottom (anus). Fistulas sometimes look like tiny pits, which may be leaking pus or poo. After an initial physical examination, you will have a further physical examination. This second examination will be done under a general anaesthetic. This is because the examination can be painful and it is helpful to have the anal sphincters and pelvic floor muscles relaxed. This is called an examination under anaesthetic or EUA. An EUA helps find out whether the fistula crosses the sphincter muscles. It also allows drainage of any abscesses.
To see where the fistula is in relation to the sphincter muscles, you may also have the following tests:
Often, a doctor will use a combination of these techniques to assess a fistula.
Bowel to bladder fistula
Doctors use a long thin telescope with a camera attached at the end to look at the bladder. They will also look at the urethra (the tube which carries pee from the bladder). This is called a cystoscopy. Camera tests to look at the gut (called endoscopy), MRI and CT are also common tests. A CT scan uses x-rays to take detailed pictures of the body.
Vaginal fistula
Sometimes, as well as MRI, ultrasound and fistulography, you might have a blue dye test. This is where the doctor inserts a tampon into the vagina and blue dye into the rectum. If the tampon stains blue, this shows that there is a connection.
Bowel to skin and bowel to bowel fistulas
Ultrasound, CT, MRI and endoscopy help investigate these types of fistula.
Treatment for fistulas involve medicines, surgery, or a combination of both. Your treatment will depend on the type of fistula you have.
Your IBD team should explain the treatment choices available to you and the pros and cons for each. Ask as many questions as you need to. Our Appointment guide has examples of questions you can ask. If you are already taking steroids, your doctor may tell you to stop. This is because steroids can increase the chance of an infection or abscess and the need for surgery.
Anal fistulas
We know more about the treatment of anal fistulas than other types of fistulas.
Medicines
Surgery
Around 2 in 3 people with Crohn’s who have an anal fistula will need an operation at some point. The aim of surgery is to heal the fistula while avoiding damage to the anal sphincter muscles.
The type of surgery you’re offered will depend on:
If you have any abscesses, these will be drained before surgery.
Seton insertion
Setons are soft surgical threads. Surgeons will pass setons through the opening in the skin, along the track of the fistula, and out the bottom. The seton is then tied to form a loop. The ends hang out of your bottom, allowing the pus and infection to drain away. The seton is usually left in for several weeks and removed if the fistula is healing. Some people say a seton feels like having a rubber band hanging out of your bottom. After a few days they no longer notice it’s there. Inserting a seton before giving infliximab leads to better results. In some cases, setons are a long-term treatment if your fistula is unlikely to heal.
It is quite embarrassing to tell someone that I have a little rubber band coming out of my bum (a seton). But I only tell people I trust and feel comfortable with, and they have been really supportive.
Finlay, age 23
Living with Crohn's
Setons are the most common surgical procedure for a fistula. There are other surgical options, but these won’t be offered to everyone. These options include fistulotomy, advancement flap, LIFT and VAAFT. Results can often be worse for complex and ongoing fistulas.
Fistulotomy
In this operation, the length of the fistula is cut open. Imagine cutting open a cardboard tube along its length and flattening it out. This promotes healing from the base of the fistula to the surface. Healing may take anywhere from a week to several months.
Fistulotomy is only for fistulas that cross the sphincters a small amount, or not at all.
I had day surgery for an anal fistula. I was anxious before the operation as I had never had a general anaesthetic before, and the surgeon couldn’t say whether he would be able to lay it open or if I would need a seton stitch. In the end it went very smoothly and he was able to lay it open. Having the operation has made such a difference. I started to feel the benefits quickly afterwards and the relief was immense.
Lucy, age 45
Living with Crohn's
Advancement flap
The inside of the fistula is removed and the tract cleaned. The hole where the fistula joined the bowel is then covered with a flap. This flap is formed from the lining of the rectum, which is end of the bowel.
This operation is used for complex fistulas. This operation is also used when fistulotomy would carry a high risk of losing bowel control.
LIFT (Ligation of Intersphincteric Fistula Tract)
This operation aims to avoid cutting the sphincter muscle. The surgeon accesses the space between the internal and external anal sphincter muscles. This is done through a small cut at the entrance to the bottom. Once the surgeon has found the fistula tunnel it is cut in two. Both ends are then stitched closed to stop poo getting into the fistula.
VAAFT (Video-Assisted Anal Fistula Treatment)
Using a telescope camera, the surgeon can see the fistula track from the inside. After cleaning, the fistula track is closed using an electric current. Stitches and fibrin glue can also be used. This technique also helps surgeons find extra passages running off the main fistula. These extra passageways also need treatment for the fistula to heal.
Risks of anal fistula surgery
Like any surgical procedure, surgery for anal fistulas has some risks. The main risks are:
The level of risk will depend on where your fistula is and the type of operation you have. Talk to your surgeon about the possible risks of the operation and the benefits that it can offer you. You will have an appointment with a surgeon prior to any operation.
Other treatments
Other treatments include closing the fistula with a special medical glue or paste. A plug made from materials like Gore-Tex® can also be used to cover the hole. Sometimes medical laser probes are used to seal the tract shut.
Stem cells
Stem cells might be effective in treating complex perianal fistulas in mild Crohn's. Stem cells could be useful if medicines have not worked, or someone does not want to have surgery. But this treatment is not approved for use in the NHS. This is because there is not enough evidence that this treatment is effective, and it is expensive.
Stoma formation
If other treatments have not worked, you may be offered an operation to remove the rectum. This allows the fistula to heal. The bowel is brought to the surface of the tummy as a stoma. Poo is then collected outside the body in a bag. Find out more in Surgery for Crohn's Disease.
Bowel to bladder fistulas
Less is known about the best treatment for bowel to bladder fistulas. Treatment can include a combination of:
Generally, medicines are used first to try and control inflammation. If medicines do not work, your IBD team may talk to you about the option of surgery. Surgery aims to remove the affected bowel, join up the healthy bowel and close the hole in bladder wall. This may be carried out in stages. As well as your IBD team, a specialist from the urology department may also be involved in your care.
Vaginal fistulas
Like bowel to bladder fistulas, less is known about vaginal fistulas. Treatment involves a combination of medicine and surgery. Immunosuppressants, infliximab and antibiotics may help treat the underlying inflammation.
Operations for vaginal fistulas include:
These operations can be difficult, so specialist surgeons will usually perform them. You are likely to have a team of different surgeons. These could include people specialised in urology, gynaecology and colorectal surgery.
Bowel to skin fistulas
For some bowel to skin fistulas, the fistula may close on its own. But if the fistula stays open for longer than two months this is not likely. If only a small amount of gut contents leaks out of the fistula then medicines like infliximab can be used. If lots of gut contents are leaking out it is more likely surgery is needed. Surgery for bowel to skin fistulas can be difficult. It is affected by factors such as the position of the fistula and how active your Crohn's or Colitis is. Your surgeon will remove the affected bowel, join up the healthy bowel, and then closes the fistula opening on the tummy. People with bowel to skin fistulas may need to stay in hospital for long periods of time.
For bowel to skin fistulas, your body’s fluid and salt levels are monitored and replaced if needed. Tell your IBD team or GP if the amount your fistula leaks changes from what is normal for you. They might need to assess your fluid and salt levels. A drainage bag can be positioned over the area where the fistula opens to collect any leakage. Your skin will need to be protected from the irritant effects of the gut contents, as these can injure the skin.
Some people with bowel to skin fistulas do not absorb enough nutrients from their food. They may also lose nutrients through the opening in the skin. This can be treated by a special liquid only diet. Find out more in Food.
Bowel to bowel fistulas
Bowel to bowel fistulas do not often need any treatment and they may heal by themselves. But surgery may be needed if there is an abscess or narrowing of the bowel. Here, the unhealthy bowel is removed and the fistula opening in the healthy bowel is stitched. Like bowel to skin fistulas, people with bowel-to-bowel fistulas may be low in nutrients. This can be treated by a special liquid only diet. Find out more in Food.
It’s sometimes hard for fistulas to heal completely. Unfortunately, no treatment is guaranteed to be successful. Sometimes fistulas that have closed come back. This is called fistula relapse. Around 1 in 3 people with an anal or perianal fistula have a fistula relapse.
If you’ve had an operation for your fistula, you will have a dressing over your wound. In some cases, this dressing is removed soon after your surgery. In other cases, you might need to change the dressings daily. This will depend on the procedure. Ask your nurse how to best care for your wound before you leave the hospital. Sometimes to stop the skin from healing too quickly, you might have to more your finger over the wound. This is done directly onto the skin. If you feel unable to do this a district or GP practice nurse can help. District nurses work in the community and can visit you in your home. Your IBD team, hospital team or GP can refer you to a district nurse.
Your IBD team, especially your IBD nurse, can help with practical advice. Your GP and the practice nurse may also be a good source of information about day-to-day care of your fistula.
Talk to your team about the best ways to:
Ask your nurse or doctor about the different types of dressing available. You can get many of these on prescription. If you need long-term dressings, you might be able to get a ‘Medical Exemption Certificate’. This makes NHS prescriptions free if you live in England. Prescriptions in Scotland, Wales and Northern Ireland are already free. Talk to your IBD team or GP to find out whether you are eligible.
Having a perianal fistula initially felt quite isolating and I also felt limited in what I could do. However, medication and identifying what worked for me helped me drastically. For example, I’ve found that being well hydrated and using sensitive wipes rather than toilet tissue reduces the pain associated with it.
Eunice, age 19
Living with Crohn's
Caring for your fistula
Everyday Life
Using the toilet
The sitz bath was the easiest, least painful and most effective way for cleaning myself after a toilet motion.
William, age 61
Living with Crohn's
Kits to help manage your fistula
You might want to create a kit to help manage your fistula when you’re out and about. This might contain:
If you have an abscess there’s a small risk of developing sepsis. Sepsis is also known as blood poisoning or septicaemia. This can be life-threatening. Sepsis is not common in people with a simple fistula. But it can happen where there’s an abscess that fails to drain. Sepsis happens when the body goes into overdrive in response to an infection. If not recognised and treated, sepsis can be fatal. If sepsis is detected and treated early people usually recover well.
Warning signs of sepsis include:
This is a medical emergency. Sepsis can be hard to spot but if you think you have symptoms call 999 or go to A&E.
Fistulas can be difficult to deal with and can have a negative effect on:
It may help to remember that lots of people have a fistula. Fistulas also happen in people who do not have Crohn’s or Ulcerative Colitis. For some people, living with a fistula becomes easier once they get used to the care their fistula needs.
Some people find that having a fistula impacts body confidence, sex and relationships. Our Sex and Relationships resource has more information.
Do not be afraid to ask for help. Your IBD team should be able to arrange for you to see a psychologist or counsellor, or you can refer yourself. This can help you feel more in control and able to cope better with living with a fistula. For more help see Mental health and wellbeing.
We follow strict processes to make sure our information is based on up-to-date evidence and easy to understand.
Please email us at evidence@crohnsandcolitis.org.uk if:
You can also write to us at Crohn’s & Colitis UK, 1 Bishop Square, Hatfield, AL10 9NE, or contact us through our Helpline: 0300 222 5700
We know it can be difficult to live with, or support someone living with these conditions. But you’re not alone. We provide up-to-date, evidence-based information and can support you to live well with Crohn’s or Colitis.
Our helpline team can help by:
Providing information about Crohn’s and Colitis.
Listening and talking through your situation.
Helping you to find support from others in the Crohn’s and Colitis community.
Signposting you to specialist organisations.
Please be aware we’re not medically or legally trained. We cannot provide detailed financial or benefits advice or specialist emotional support.
Please contact us via telephone, email or LiveChat - 9am to 5pm, Monday to Friday (except English bank holidays).
If you need specific medical advice about your condition, your GP or IBD team will be best placed to help.
Would you like to save the changes made to this page?
Your details were successfully saved.
