I was diagnosed with Ulcerative Colitis in 2008 at just 17 years old.
In March 2013 my condition took a turn for the worst and the idea of having major surgery and an ileostomy wasn't the most welcomed, especially at 21 years old.
Unfortunately due to the extent of my condition I had no other choice. The inflammation in my bowel was now so severe it had begun to turn toxic, the decision was either have a colostomy bag or possibly lose my life to a rupturing bowel, it was either 'a bag or a box'. I obviously choose the bag…
 I was admitted into hospital one Monday evening after having a weekend of excruciating pain. I had been living with a condition called Ulcerative Colitis of which I had been diagnosed with at 17 years old.
I was admitted into hospital one Monday evening after having a weekend of excruciating pain. I had been living with a condition called Ulcerative Colitis of which I had been diagnosed with at 17 years old.
Most people ask what Ulcerative Colitis is? Well it's a long-term condition, where the colon and rectum become inflamed. The colon is the large intestine (bowel), and the rectum is the end of the bowel where stools are stored. Ulcers can develop throughout the colon and bowels lining, and can bleed and produce pus.
The symptoms of Ulcerative Colitis aren't pleasant the main symptoms are; recurring diarrhoea which usually contains, blood, mucus or pus. Excruciating abdominal pains (tummy pain) a need to frequently empty your bowels. This can be anything from four times a day up to twenty times a day depending on the extent of your Colitis.
The severity of these symptoms varies this is dependent on how much of the rectum and colon is inflamed and how severe the inflammation is. For some people, the condition has a significant impact on their everyday lives.
Some people may go for weeks or months with very mild symptoms, or none at all this is known as remission, followed by periods where the symptoms are very troublesome these are known as flare ups or relapses.
What is the cause of Ulcerative Colitis? It is thought to be an autoimmune condition. This means the immune system (the body's defence against infection) goes wrong and it attacks healthy tissue in other words it begins to attack itself.
The most popular theory for UC is that the immune system mistakes harmless bacteria inside the colon for a threat and attacks the tissues of the colon, causing it to become inflamed.
Exactly what causes the immune system to behave in this way is unclear. Most experts think it is a combination environmental and genetic factors.
 Those who tend to be affected by Ulcerative Colitis are usually youngsters aged between 15-25 years old although this isn't always the age group, currently it is the most common age group to be diagnosed.
Those who tend to be affected by Ulcerative Colitis are usually youngsters aged between 15-25 years old although this isn't always the age group, currently it is the most common age group to be diagnosed.
It is now estimated that around 1 in every 420 people living in the UK has Ulcerative Colitis; this is around 146,000 people but the reason for WHY we have Ulcerative Colitis is still unclear. Ulcerative Colitis is a chronic condition and by this it means that it cannot be cured and it is a life long illness BUT it can be controlled by taking medication.
Treatment for Ulcerative Colitis aims to relieve symptoms during flare ups and to prevent long-term symptoms from returning which is known as remission during remission medication is used to maintain it. Most people, achieve remission by taking medication such as immune-suppressants, steroids or chemotherapy drugs all of which can be tough on the individual receiving the treatment, I personally had a lot of difficulty with maintaining remission on medication and unfortunately suffered many other horrible side effects.
Mild to moderate flare-ups are usually treated at home which usually involve medication and rest. However, more severe flare-ups need to be treated in hospital to reduce the risk of serious complications, such as gas becoming trapped inside the colon, which can lead to severe bloating.
If medication is ineffective at controlling symptoms, or quality of life is significantly affected by your condition, surgery to remove your colon may be an option. My condition unfortunately reached this point and I was admitted as an emergency patient, the colorectal surgeon on call that evening decided that we had ran out of options and the only option left was to remove my large intestine and my colon.
During my surgery, my small intestine was diverted out of an opening in my abdomen (an ileostomy) I lived with my ileostomy from March 2013 through until November 2013 where I then underwent surgery to create an internal pouch this is connected to the anus and the medical term is known as an ileo-anal pouch during this surgery my pouch was formed but I am still waiting for my pouch to be connected so at present I am still living with an ileostomy although it has just been confirmed that I am due to undergo 'take down surgery' in other words stage 3 and hopefully my final stage on 5th November.
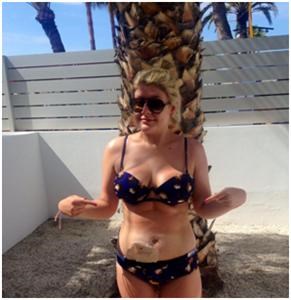
People often ask how I have coped with going through so much surgery at such a young age, my response to this is that it was a bag or a box, the lifestyle I have since having an ileostomy is AMAZING I will be sad to see my ileostomy go as it has given me six years of my life back, I can socialise with friends in public again, go out for dinners, go on holidays and make it at least 4 hours without having to set foot in a bathroom.
 Living with the ileostomy itself has become relatively easy over time, initially there is the fear of having a stoma (a small piece of intestine which passes waste into a colostomy bag) initially it can make you feel slightly squeamish as its on your body but it doesn't hurt or have nerves and it is easy to maintain on a daily basis.
Living with the ileostomy itself has become relatively easy over time, initially there is the fear of having a stoma (a small piece of intestine which passes waste into a colostomy bag) initially it can make you feel slightly squeamish as its on your body but it doesn't hurt or have nerves and it is easy to maintain on a daily basis.
I personally take care of my ileostomy each day by changing my bag each morning once I get out of the shower the bags don't have to be changed daily it can be done weekly but for my own piece of mind I prefer doing mine on a daily basis it has become routine for me. The bag is removed using adhesive remover, it is then cleaned by using gaze or antiseptic wipes especially made by healthcare companies I then dispose of my used bag by putting it into a nappy sack which masks any smells, I then cut my bag to fit the size of my stoma and stick it to my skin.
The process of changing my bag usually takes anything from 2-5 minutes. I always carry extra supplies when going out for the day or when travelling somewhere in case of a leak -these are very rare, I also carry a set of spare clothes with me if I am flying somewhere or going on a long road trip, it personally gives me peace of mind to have my emergency kit handy.
My medical supplies are sent to my door whenever I request them I simply order these online via a healthcare company -there are many out there to choose from the company then sort the prescriptions out through my GP.
A tip for ileostomy users is make sure you speak to your GP to issue you a 'Medical Exception Certificate' as the stoma (ileostomy) is a permanent fixture until a reversal or if you choose to keep it for life you are medically exempt from paying prescription charges for ileostomy supplies, medication etc. I wasn't told this by my GP so I would recommend those who have ileostomy's to speak with their consultant or GP. I also see my stoma nurses on a monthly basis this is just to check that my stoma is ok as occasionally the skin can become sore as it is an open wound. I can still go swimming with my bag, I can shower and I have even skydived!
Since having the surgery I have been given my life back throughout my teenage years I suffered with side effects from medication and never fully going into remission so having surgery was literally an absolute life saver. I have friends and family who say that I am much more positive since having surgery and the old bubbly me is back I am now campaigning to raise as much awareness as I can on Ulcerative Colitis and Crohn's Disease.
I am forever thankful to the charity, Crohn's & Colitis UK, who have helped and supported me from day one. I do really hope and think that the 'taboo on poo' is slowly beginning to be broken as more of us fighters are beginning to speak out about these debilitating diseases we just need to see more funding go into charities like Crohn's & Colitis UK to try and find a cause or a cure to keep more of us in remission.
My words to those newly diagnosed are; don't suffer alone, use the support groups available via Facebook, twitter and also local support groups within your area which can be found on the Crohn's & Colitis UK website. I personally always use the phrase 'break the taboo on poo' there is such a stigma around bowel related illnesses and this really needs to go away as the more people talk about these conditions the more awareness can be raised and also more people can be diagnosed earlier giving more treatment options.
Always get checked out by your GP if you notice any blood in your stools it might be nothing severe but it's always worth getting checked out remember that there is no shame and its nothing that a GP hasn't dealt with before leave your dignity at the door.
Patients who are newly diagnosed should visit the information section of the Crohn's & Colitis UK website. At 17 when I had just had my confirmed diagnosis I read the help sheets on the webpage from then onwards any answers I needed I found on the webpage and also by becoming a member on the Facebook page where I have been able to share stories with other sufferers and together we have all built a great support network along with great friendships.

Personally for me having the Crohn's & Colitis UK forum was a lifeline to put me touch with others in the same position as me and the relief of knowing that I wasn't the only person my age going through this disease alone.
I do really hope with more patients speaking out through social media that there is hope for 'US' as a group of individuals to finally get outsiders to understand how tough IBD really is and how much all of us sufferer on a daily basis.
Together we will #breakthetaboo.

