Patient Involvement in Research Day 2022

The IBD Patient Involvement in Research Day held on Saturday 15th October 2022 was a great success, with 141 attendees joining us on Zoom to share their views and take part in shaping research.
We heard from IBD researchers at the top of the field, pioneering new research, and providing participants with the opportunity to choose from a range of focus groups and workshops to speak directly to researchers and help them shape their projects.

Want to catch up?
You can view part 1 of the event below.
Patient Involvement in Research Day 2022 Timestamps:
00:00-3:52: Welcome and Introduction from Ruth Wakeman, Director of Services, Advocacy and Evidence, Crohn's & Colitis UK, and Dr Jackie Craissati, Chair of Board of Trustees, Crohn's & Colitis UK.
3:52-27:52: Overview and Q+A of Current IBD Research Landscape from Professor Shaji Sebastian, Chair of the British Society of Gastroenterology Research Committee and IBD Service Lead at Hull University Teaching Hospitals.
27:52-46:33: Personalised Medicine and Q+A with Dr Matthias Friedrich, Kennedy Institute of Rheumatology and Translational Gastroenterology Unit, University of Oxford, and Ruby Bryant, talking about lived experience.
46:33-1:06:50: Psychological and Biological Profiles of Chronic Pain in Patients with IBD and live poll, with Pavit Luthra, Gastroenterology Registrar, Queen Mary University of London.
1:06:50-1:19:47: Patient and Public Involvement Case Study in Stoma Product Design with Toni Schneider, Ostique.
1:19:47-close: Summary and thanks from Ruth Wakeman, Director of Services, Advocacy and Evidence, Crohn's & Colitis UK, and Dr Jackie Craissati, Chair of Board of Trustees, Crohn's & Colitis UK.
Find out about the workshops
We ran 8 workshops on the day. Scroll down to find out what each one was about by watching a pre-recorded video, or reading a short summary. We will be sharing feedback on these focus groups in due course.
IBD-BOOST: how should we share the findings of our national fatigue, pain and urgency study?
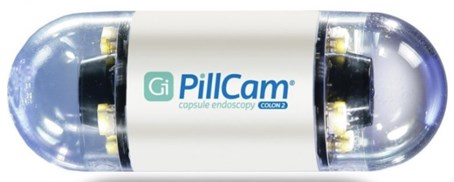
Artificial Intelligence in capsule endoscopies (pill cameras)
Artificial Intelligence (AI) is now being used to make a diagnosis at endoscopy. During the recent Crohn's & Colitis Patient Involvement in Research Day, patients with IBD were invited to take part in a workshop focused on their views of using AI at diagnosis.
The discussion aimed to explore whether patients would feel comfortable with AI in making a diagnosis as opposed to a trained clinician viewing capsule footage.
Feedback gained highlighted that patients wanted to be completely sure of the diagnostic accuracy of AI. Furthermore, they expressed concerns that without a clinician reviewing footage the human element of care was missing. They also wanted to ensure that if AI was adopted that lesions were not missed by the computer-based algorithm and that there was no risk of over diagnosis which would lead to treatment being commenced which would not be necessary.
The positives raised for the use of AI were centered on the fact that a computer-based diagnosis could prove to be more productive and avoid delays in diagnosis making and treatment being started, particularly at a time where healthcare staffing is proving to be an issue. And that with a computer-based diagnosis at capsule endoscopy one could assess response to treatment more easily through simple swallowing of a small device as opposed to undergoing a colonoscopy which could prove more uncomfortable.
Scottish Gut Project – the link between arts, communication and language in gut disorders and wellbeing
Engaging people with IBD in mental health research
Your views on the future of Personalised Medicine and increasing engagement
The aim of our study is to bring personalised medicine for people with Crohn’s and Colitis one step closer. Personalised medicine is when treatment is tailored to individuals.
There is currently no cure for Crohn’s or Colitis. People living with the conditions experience unpredictable periods of relapse, known as ‘flare-ups’, and remission. Medicines can help in many cases, but not all. Some people do not respond to any medicines, and surgery may be needed to remove inflamed bowel sections. All this can have a big impact on people’s quality of life, mental health, and wellbeing.
Recommended treatments include medicines called ‘biologics’. Biologics aim to get symptoms under control and keep them under control. These medicines work by blocking the proteins, called cytokines, that ‘switch-on’ inflammatory responses. This, in turn, reduces inflammation. Biologics are now the most prescribed treatment for Ulcerative Colitis. There are many different types, each targeting a different inflammatory protein. For some people, a particular biologic may help reduce inflammation and control symptoms, but for others it does not. Some people need to try several biologics before they find one that works for them.
Our research is being shaped by people with lived experience (both Crohn’s and Colitis) and will investigate bowel inflammation at a microscopic and molecular level. Specifically, the project will explore ways to match individuals with Ulcerative Colitis to the medicine that will work best for them. This will mean that their symptoms are controlled more quickly and they have a better quality of life.
When we recently used a microscope to look at tissue samples taken from people with Ulcerative Colitis, we found that different cells and molecules contribute to disease in different people, so bowel inflammation is individual to each person. Despite these differences in the features of the disease, biologics are prescribed in a ‘one-size-fits-all’ way. This approach does not consider the individual molecular characteristics of the person’s bowel inflammation at the time of treatment. By targeting treatment according to the individual’s molecular pattern, our research aims to decrease the failure rates of current treatments and bring us much closer to personalised medicine for Ulcerative Colitis.
In this focus group, we asked participants for thoughts on whether you would be willing to try a personalised medicines approach – if proven successful first – in a clinical trial setting. We would also discussed ideas on how patient engagement groups can get more involved in research.

Schematic overview: Decades of research have helped us to find molecules that can be targeted by medications to stop or reduce intestinal inflammation. Similarly we recently found that that certain molecular signatures of inflammation are reflected on microscopic images already taken for diagnostic purposes in hospitals. The studies we are conducting together with patient engagement and Crohn’s & Colitis UK are aiming to find out whether either molecular signatures or microscopic images – or both – can be used to better tailor medicines to individuals.
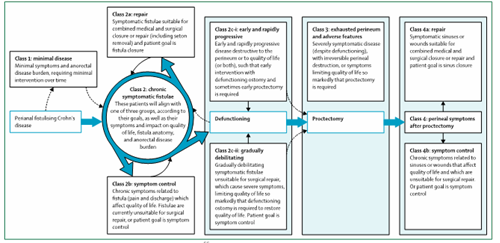
Creating Better care for People with Perianal Crohn's Disease
Perianal fistulising Crohn’s Disease is an aggressive type of Crohn’s that can significantly impact people’s quality of life. Current scientific understanding of perianal fistulising Crohn’s Disease needs to be improved. Previous classification systems have not helped doctors to choose the right treatment for individuals with fistulising Crohn’s Disease, nor have they guided how we best group people in clinical trials. We have developed a new classification system for perianal fistulising Crohn’s Disease to address this unmet need, to consider people’s symptoms and individual needs along with best practice clinical management.
Our proposed classification system puts people with perianal Crohn's into different groups based on their fistula symptoms and personal treatment goals. Going forward, we aim to then include best practice management within each of these groups. We understand everyone with perianal Crohn's is different in the way the condition affects their quality of life and symptoms. Therefore, it is important our classification considers different patient journeys within the groups we are suggesting.
In our focus group, we discussed this proposed new classification system with people living with perianal Crohn’s to see what they think of it.
Click on the image below to view a full-size version
Resource use, quality of life and value of self-management in IBD
Scope of research work
We have designed a survey to estimate the economic burden of IBD on people living with Crohn's and Colitis (the financial impact on an individual caused by their condition). Our aim is to estimate the cost of care and the loss of work, income or productivity of people with IBD in the UK and to identify which aspects of IBD and its treatment, lead to the most costs for the individual.
We hope that the results of this study will inform policy makers and help them to better use NHS resources to manage IBD in the UK.
About the survey
Study setting and participants
The data will be collected via surveys that can be completed by individuals online or via a paper copy. We will recruit from 2 sources:
- The IBD BioResource: currently with over 35,000 participants with confirmed IBD recruited from NHS outpatient Gastroenterology clinics across the UK.
- The Royal London NHS Hospital IBD Clinic: we will recruit 150 patients through the IBD clinic. Most IBD patients are under the care of a gastroenterologist.
Eligibility criteria
All adults over 18 with a diagnosis of IBD, living in England, Scotland or Wales, able to give informed consent and to complete a written survey in English are eligible for inclusion in the study.
Study size
We will approach 8,700 people with IBD, and we hope to receive completed surveys from 2,000 participants over a 6-month period.
Survey sections
The Survey will include the following sections to be completed by the participant:
- Demographics and lifestyle behaviour
- Disease history and health
- Crohn’s or Colitis activity
- Disease control from the patient's perspective
- Quality of life measurement
- Questionnaire on resource use
- Employment details
- Work productivity and activity impairment
The focus group
During the focus group we discussed:
- The overall survey (clarity, length, relevance of questions, ethical considerations)
- Making sure a wide variety of people complete the survey, so we can understand the experiences of people from different backgrounds and with different forms of IBD
- Your ideas on how we can approach patients and offer them the chance to complete the survey while waiting for their medical appointment
- How this survey may be helpful to people with IBD
- Your thoughts on how we should share the research findings and the input of our PPI (Patient and Public Involvement) group
- Any other questions / suggestions you may have
Innovation in IBD colorectal cancer surveillance
It was good to hear that there was an overall agreement to develop a more precise way of assessing risk using clinical data, including previous endoscopies and tissues samples, which are collected during routine care.
During the focus group, Dr Din and the participants discussed the importance of surveillance to detect bowel cancer early in patients at risk with IBD affecting the large bowel (colon).
Currently, routine non-invasive stool tests are used help prioritise colonoscopy timing to manage the backlog created by the COVID-19 pandemic.
For many reasons, surveillance has not been as successful as envisaged, improvements are needed to predict the level of risk for each individual patient.
During the colonoscopy, doctors search for subtle abnormalities in the lining of the bowel, which can be harder to detect if there is obvious inflammation at the time or the bowel preparation has not worked so well.
Each colonoscopy is an opportunity to look for the early changes of cancer although many times this will not be possible as the time allocated to a standard colonoscopy is shorter than a surveillance procedure which takes longer.
Collecting additional saliva, blood, stool and tissue samples during procedures would also be acceptable and more convenient if they could be integrated into regular appointments such as infusion treatments to minimise any additional travelling (which also supports environmentally sustainable efforts).
Many also believed that there are missed opportunities for aligning research with the regular care that is provided, and most patients are often happy to provide additional samples if this would help provide better overall care.
Participants discussed the use of clinical data in more general terms and how healthcare and research data is heavily regulated and protected, accessed by healthcare professionals involved in your care or approved researchers.
The focus group broadly agreed that colonoscopy is an invasive test and targeting colonoscopy based more precisely on individual risk more seemed to be a good idea.
This approach may lead to some patients having more or less surveillance procedures in the future.
Helpline
Service
We know it can be difficult to live with, or support someone living with these conditions. But you’re not alone. We provide up-to-date, evidence-based information and can support you to live well with Crohn’s or Colitis.
Our helpline team can help by:
-
Providing information about Crohn’s and Colitis.
-
Listening and talking through your situation.
-
Helping you to find support from others in the Crohn’s and Colitis community.
-
Providing details of other specialist organisations.
Please be aware we’re not medically or legally trained. We cannot provide detailed financial or benefits advice or specialist emotional support.
Please contact us via telephone, email or LiveChat - 9am to 5pm, Monday to Friday (except English bank holidays).
If you need specific medical advice about your condition, your GP or IBD team will be best placed to help.