Eating and drinking
After your surgery, you may have to change what you eat for a short time. Your surgical team will give you specific advice on what you should eat. For example, they may advise you to eat a diet low in fibre. This will make it easier for your gut to break down and absorb food while it recovers from surgery.
As you recover, you may find that you can eat larger meals and a wider range of foods.
Most people with a stoma do not need to stay on a special diet. But there might be some foods or drinks that make your stoma more active or give you bad gas. This is different for everyone. Your stoma care nurse or the hospital dietitian should be able to advise you.
You can see our information on food for more on diet and Colitis. Or see our information on life with a stoma for specific information on eating with an ileostomy.
Hydration
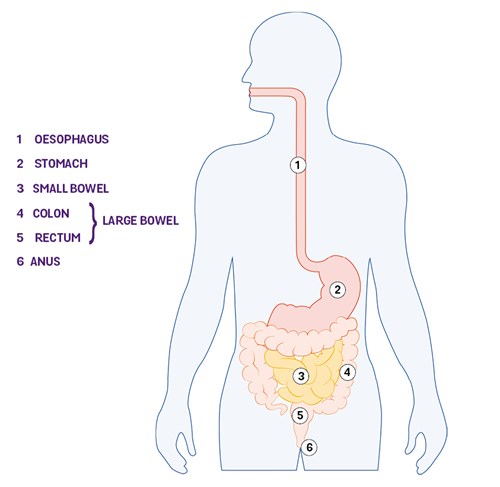
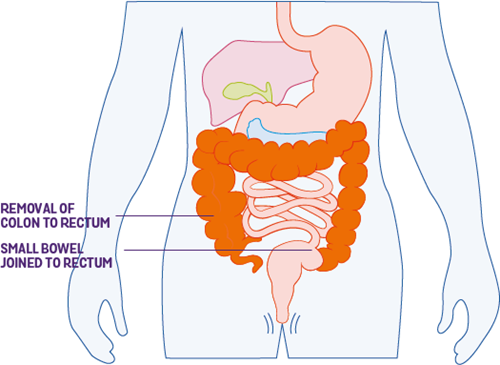
Your colon, part of your large bowel, is important for absorbing water. If you have your colon taken out, you have a higher risk of dehydration. You may find it helps to drink extra fluids and rehydration drinks, including electrolyte mix. You might find our information on dehydration helpful. Our information on life with a stoma also has information on staying hydrated with a stoma.
Emotional reactions
Everyone reacts to surgery in their own way. And it’s important to remember there is no right or wrong way to feel.
As you go through the process of needing and having surgery, your emotions may change. Emergency surgery can be especially difficult as there is less time to adjust. Throughout this time, you may feel worried, scared or maybe nervous. You may feel a sense of relief. Or, if you chose to have surgery, you may doubt whether you made the right decision. Try and be kind to yourself, and recognise you are going through a lot. Take time to look after yourself and do not be afraid to ask for help if you need it.
Going through lots of different emotions can be exhausting. You may find it helpful to talk to someone about these feelings. IBD nurses, stoma nurses and psychologists can all help to support you. You can also speak to your GP about local mental health support. Our information on mental health and wellbeing has further details about this.
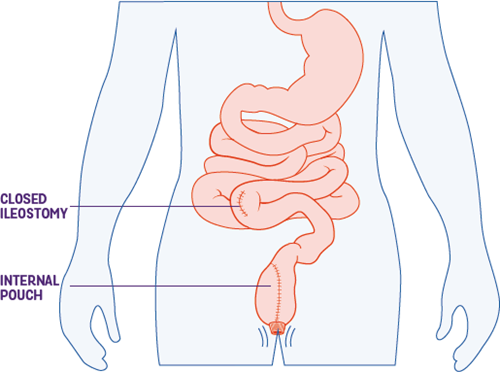
Some people find it helpful to talk to someone else who has been through surgery. The Ileostomy & Internal Pouch Association provide trained peer support volunteers who you can talk to.
People close to you may also find it difficult to cope with the thought of you having surgery. Our information on supporting someone with Crohn’s or Colitis might be helpful in supporting them and their emotions.
Driving
In the long term, surgery should not affect driving. However, you may have to avoid driving straight after surgery. You should not drive again until you are able to control a car properly, including making an emergency stop if needed. This may take several months. If you still cannot drive safely three months after your surgery, you need to tell the Driver and Vehicle Licensing Agency (DVLA). Your car insurance may not cover you if you drive before you are fully recovered, so check the terms of your policy. It may be helpful to ask your surgeon to confirm that you can drive again in writing, at your follow-up appointment.
Work and finances
If you work, you may wonder how surgery will affect your job and your income. It can take time before you feel able to return to work. For some people this might mean three weeks, but for others, it is more. Some surgeons will sign you off for six weeks as standard. How long you will need off work will depend on the type of surgery you’re having and the type of job you have. If you work in a very physical job, you may need more time off.
If you can, it’s best to let your employer know early on about your medical needs and time off so they can make adjustments. It may help to read our information on employment.
If you are absent for more than a week, you will need to get a ‘fit note’ from the healthcare professional who is caring for you. They can make suggestions for additional support or adjustments when returning to work. This could include building up slowly to your usual working hours and duties. This is called a ‘phased’ return to work.
See the Advisory, Conciliation and Arbitration Service (ACAS) website for more information on returning to work after an absence.
If you’re worried about money, have a look at our information on money and finding financial support. You may be eligible for support. You can also visit the UK Government website or Citizens Advice for more information on welfare benefits. If you care for a child who lives with Colitis, you may want to read our information on disability benefits for children to see you if are eligible for financial help.
Sex and relationships
You may be worried about how surgery will affect your sex life. Your surgical team can give you specific advice about when they think it’s safe for you to have sex after surgery. Going back to sexual activity may mean exploring other ways of being intimate or new positions. It can be difficult to talk about sex, but being open about your needs and concerns can help.
Some people who have surgery for Colitis may not be able to have anal sex. This will depend on the surgery you have. We have separate information about this in sex and sexual health.
For some men, having surgery may lead to difficulties with erections. This issue may go away by itself. But if not, speak to your IBD team or GP for ways to help.
Our sex and sexual health information has more on how surgery may affect sex and suggests other ways you could be intimate with a partner.
Body image
Your body may look different after surgery, and you may find this difficult to come to terms with. On the other hand, you may feel that having surgery improves your body confidence. You may feel better and able to do the things you enjoy. Maybe you can start going to the gym. If you’re having worries, talk to your IBD team.
Your nurses will likely have spoken to lots of people about their body image worries. It may also be helpful to speak to others who have been through a similar experience. Check our support for you page for ways you can connect to others living with Crohn’s or Colitis. Our information on mental wellbeing may also be helpful.