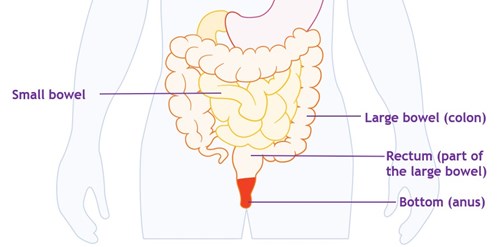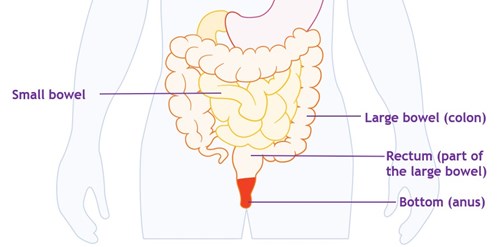
The bowel is the largest part of your gut. It consists of two sections, the small bowel and the large bowel. You might also hear them called the small intestine and the large intestine. The large bowel consists of the colon and the rectum. The rectum is the part that stores poo.
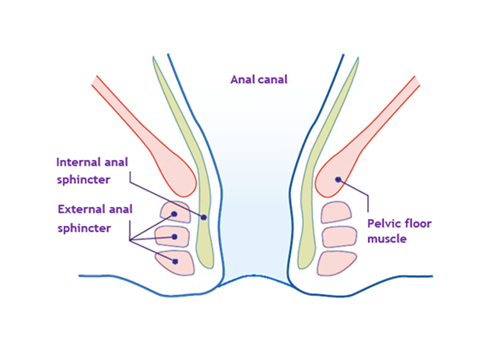
At the end of your rectum is the anus. This is the opening where poo comes out of your bottom. The anal canal connects the rectum to the anus. The way your body controls when you fart (pass wind) and poo is complicated. It involves:
- The ability of the rectum to keep poo in
- The muscles of the bowel, rectum, and anus
- Nerve signals from the bowel to the brain
If any of these systems are not working as well as they should, you may experience urgency or bowel incontinence.
The most common causes of bowel control problems for people with Crohn’s or Colitis are:
Diarrhoea
Diarrhoea (passing a looser poo more often than is normal for you) is a key symptom of Crohn’s and Colitis. It can be difficult for the rectum to hold in liquid poo, especially when it happens often. So, urgency and bowel incontinence can develop.
Inflammation of the bowel
In a healthy gut, the muscles in the bowel move poo slowly along the bowel. In people with Crohn’s or Colitis the bowel can become inflamed, which makes it more sensitive. This can make the rectum more active, pushing poo out as soon as it arrives. Inflammatory changes to the muscles and nerves of the gut can persist once inflammation dies down. This can cause problems with bowel control even when disease is not active.
Muscle damage
Muscles in your bottom (anus) work to keep poo in until you are ready to pass it. These muscles are known as your anal sphincter. If these muscles are damaged, you may have less control over passing wind, and liquid or solid poo. In people with Crohn’s or Colitis, these muscles can become damaged by:
- An anal fistula
- Pouch surgery
- Perianal surgery
Damage to the muscles can also be due to other causes not related to Crohn’s or Colitis. These include childbirth, surgery, or piles (haemorrhoids).
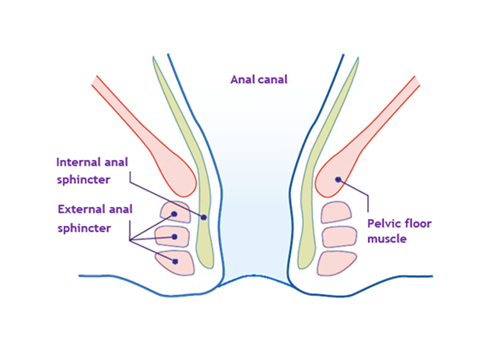
This diagram shows the position of the muscles around the anal canal where poo travels. The pelvic floor muscles also help you control when you pass pee, poo, and wind.
Nerve damage
Nerves control both the sensations from the bowel, and the anal sphincter muscles. Ongoing inflammation due to Crohn’s or Colitis can affect the nerves in the gut lining. This damage can make the bowel more sensitive and affect control of the anal sphincter.
Constipation
Some people with Crohn’s or Colitis have constipation. Constipation is when it becomes difficult to poo, and you may not have a poo for several days or even weeks. When you do it may be hard and lumpy. Liquid or solid poo can build up in the large bowel and become packed together. Liquid poo can then sometimes leak around the packed poo. This is sometimes called overflow diarrhoea. You might not be aware of this leakage, as there will be no urge to have a poo.
Perianal fistula
A fistula is when a narrow tunnel develops that connects an organ to another part of your body. A perianal fistula connects the anal canal or rectum to the surface of the skin near your bottom. Pus, blood, or poo can drain from the fistula opening. A perianal fistula can also cause damage to the anal sphincter. See our information on Fistulas for more details.