At first, the aim of treatment is to reduce the inflammation in your gut and get your symptoms under control (remission). This is called induction treatment. Once your symptoms are under control, treatment aims to keep it under control. This is called maintenance treatment.
Find out more about how we talk about the effectiveness of medicines.
Colitis
5-ASAs work well at getting and keeping symptoms under control in people with Colitis. But they do not always work for everyone – what is right for one person, may not be right for someone else.
Getting Colitis under control
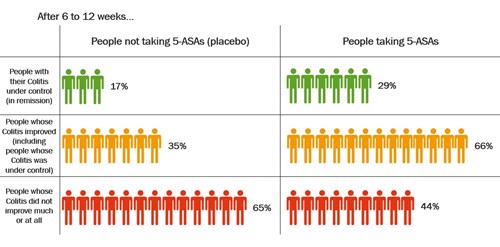
A review of studies looked at how well 5-ASAs can get symptoms of Colitis into remission. The review combined data from studies that compared 5-ASAs with a dummy treatment (placebo). The 5-ASAs in these studies were given by mouth. The review found that 5-ASAs worked better than placebo to get Colitis under control.
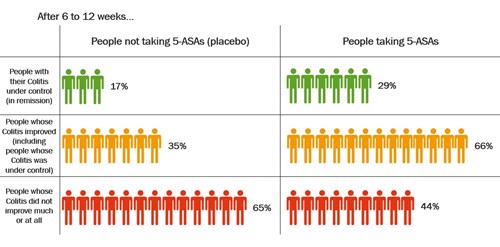
Click to view at full size
After 6 to 12 weeks, more people had their Colitis under control (in remission) after taking a 5-ASA compared with people who had not been taking a 5-ASA (placebo). About 29% (29 in every 100 people) who took a 5-ASA had their Colitis in remission compared with 17% (17 in every 100 people) who took placebo.
Keeping Colitis under control
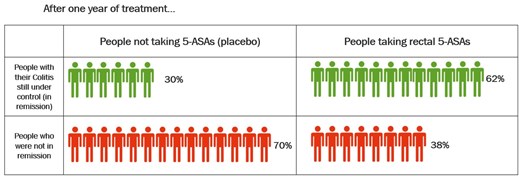
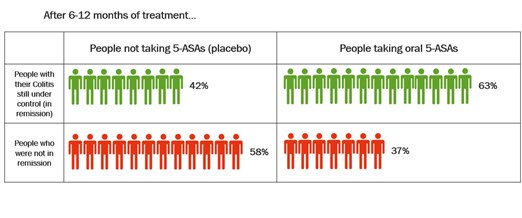
Two reviews have looked at how well 5-ASAs keep symptoms under control in people with Colitis. These reviews combined data from studies that compared 5-ASAs with a dummy treatment (placebo). One looked at rectal 5-ASAs, which you insert into your bottom. The other looked at oral 5-ASAs, which you take by mouth. The reviews found that 5-ASAs worked better than placebo to keep Colitis under control.
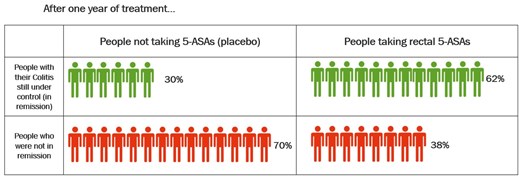
Click to view at full size
After 1 year, more people had their Colitis in remission after taking a rectal 5-ASA compared with people who had been taking placebo. About 62% (62 in every 100 people) who took a rectal 5-ASA had their Colitis in remission compared with 30% (30 in every 100 people) who took placebo.
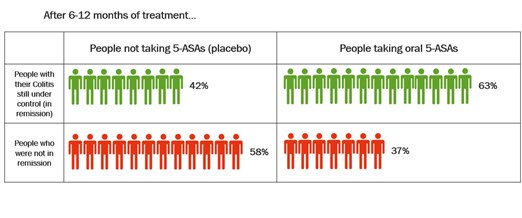
Click to view at full size
After 6 to 12 months, more people had their Colitis in remission after taking an oral 5-ASA compared with people who had been taking placebo. About 63% (63 in every 100 people) who took an oral 5-ASA had their Colitis in remission compared with 42% (42 in every 100 people) who took placebo.
Crohn’s
Getting Crohn’s under control
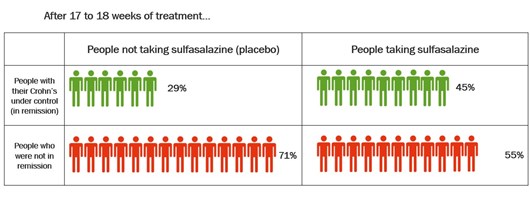
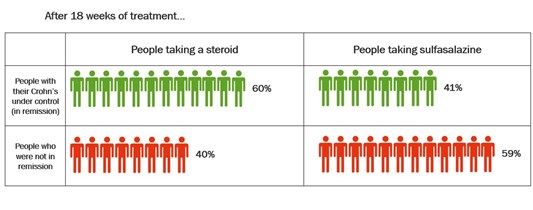
A review of studies looked at how well 5-ASAs can get symptoms of Crohn’s into remission. The review combined data from studies that compared 5-ASAs with a dummy treatment (placebo). It found that sulfasalazine provides a small benefit for people with mild to moderate Crohn’s. But sulfasalazine did not work as well as steroids. Mesalazine was not effective for inducing remission in active Crohn's.
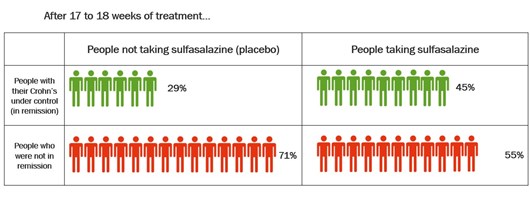
Click to view at full size
After 17 to 18 weeks, more people had their Crohn’s in remission after taking sulfasalazine compared with people who had been taking placebo. About 45% (45 in every 100 people) who took sulfasalazine had their Crohn’s in remission compared with 29% (29 in every 100 people) who took placebo.
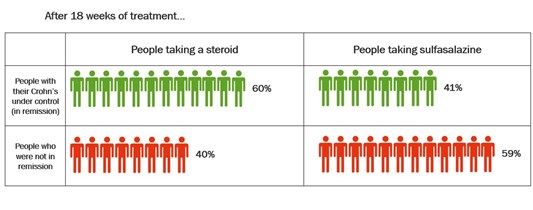
Click to view at full size
After 18 weeks, more people had their Crohn’s in remission after taking a steroid compared with people who had been taking sulfasalazine. About 60% (60 in every 100 people) who took a steroid had their Crohn’s in remission compared with 41% (41 in every 100 people) who took sulfasalazine.
Keeping Crohn’s under control
Medically-induced remission
A review looked at how well 5-ASAs keep symptoms under control in people with Crohn’s who had received medicines to get their symptoms under control (in remission). This review combined data from studies that compared 5-ASAs with a dummy treatment (placebo). It found that 5-ASAs were no more effective than placebo for maintaining remission achieved by medical treatment.
Surgically-induced remission
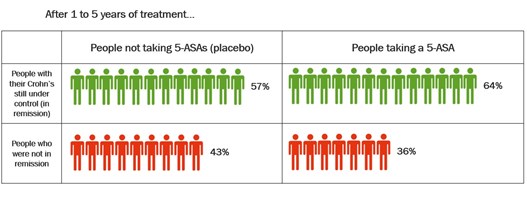
Some people with Crohn's will need surgery to get them into remission. A review looked at how well 5-ASAs keep symptoms under control in people with Crohn’s who had surgery to induce remission. This review combined data from studies that compared 5-ASAs with a dummy treatment (placebo). It found that 5-ASAs were slightly more effective than placebo for maintaining remission in people with Crohn’s.
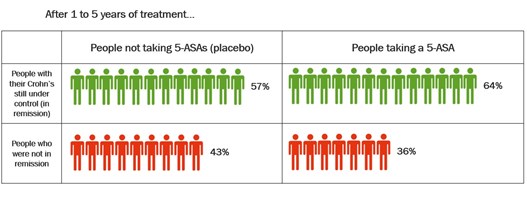
Click to view at full size
After up to 5 years of treatment, slightly more people continued to be in remission after taking a 5-ASA compared with people who had been taking placebo. About 64% (64 in every 100 people) who took a 5-ASA continued to be in remission compared with 57% (57 in every 100 people) who took placebo.