This information is for people with Ulcerative Colitis who are taking or thinking of taking filgotinib. Filgotinib is also known by the brand name Jyseleca.
This information can help you decide if filgotinib is right for you. It looks at:
- How filgotinib works
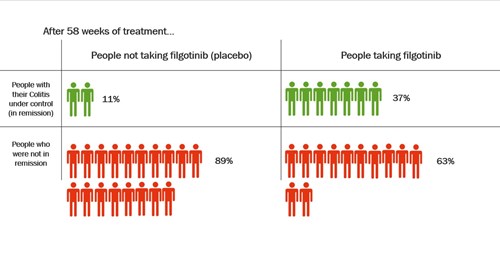
- How well filgotinib works
- Why you might be offered filgotinib
- What you can expect from filgotinib treatment
- Possible side effects
- Stopping or changing treatment
Where we use ‘Colitis’ in this information, we refer to Ulcerative Colitis only.
This information might use words you have not heard before. Our page on medical words can help provide an explanation.