Connect with other children
Children may feel less isolated if they can talk to others in a similar situation. You may be able to meet other families through the Crohn’s & Colitis UK Local Networks and events across the UK. The charity CICRA has an E-Pal scheme, which gives children a chance to chat with other children with Crohn’s or Colitis.
Get them involved
There are lots of things about Crohn’s or Colitis that your child cannot control. But you can give them choices about their care, when possible. This can help them feel more in control. For example, which arm they’d prefer the needle in, or what they’d like to do after taking their medicine.
Show them simple ways to manage their condition. Younger children could put on their own ‘magic cream’ to numb their skin before blood tests, or their own plaster afterwards. Older children could gradually have more responsibility for managing their own medicines.
Use play to ease fear and anxiety
Try taking a doll or teddy along for blood tests. It could help to pretend that the toy is a patient and use it to explain what will happen.
Children’s nurses at the hospital are often used to encouraging this type of play. But appointments at the GP surgery are often shorter, and the practice nurses may have less time to prepare your child or use toys. In this case, it may help to arrive early so that you have extra time to play and prepare your child while you wait.
Help them see the funny side of things
At times, having a sense of humour could help your child feel better. It might help them realise that their symptoms are not embarrassing. Some parents tell us that it’s good to laugh about things, as long as the child feels comfortable and does not think you are laughing at them.
Get professional help if you’re worried
If you’re worried that your child is not coping with their diagnosis, it may help them to talk to a psychologist or counsellor. Their IBD team might be able to help with this.
Your child’s emotional wellbeing
Your child will experience ups and downs, just like any other child. But you might notice more worrying changes in their mood or behaviour at times. Signs they may be struggling include:
- Sadness or a low mood that does not go away
- Being irritable or grumpy all the time
- Not being interested in things they used to enjoy
- Avoiding time with friends and family
- Having trouble sleeping, or sleeping more than usual
- Behaviour changes at school or at home
Encouraging your child to talk is an important first step. They may find this difficult, so keep trying and stay positive and encouraging. Make sure they know that you want to listen and choose a time when there are few distractions. Younger children may find it easier to draw what’s worrying them. Teenagers may be more likely to open up if you’re side by side, for example sitting in the car or going for a walk.
Your child may find it easier to talk to another trusted adult, such as a close family member, someone in their IBD team, or their favourite teacher. Whoever your child chooses to talk to, discussing their worries can help them to see things differently and find ways to cope.
Parents and healthcare professionals have found several ways to support children’s emotional wellbeing. There may be something here that could help your child:
- Write down how they feel or keep a mood diary. Older children could try the NHS recommended Kooth app, which has a space for keeping a journal. They can also get support from other young people and professionals through the app.
- Do what makes them feel relaxed, like watching a film, reading a book or playing a game.
- Younger children may find it helpful to act out their feelings with their dolls or cuddly toys. You can then help them to think of ways to make their toys feel better.
- Teenagers could try the NHS recommended Tellmi app. This is a safe space to open up and get positive advice and support from other young people. All posts and replies are checked to make sure the comments are kind.
- Practise deep breathing, meditation or yoga. Apps or YouTube videos can guide them through these techniques.
- Go for a walk, take part in sports or exercises they enjoy, or try something new.
- Try painting, colouring, or another type of craft.
If you’re concerned about your child’s emotional wellbeing, talking to a counsellor might help them. Check if your child’s IBD team has a counsellor or clinical psychologist or ask if they can refer your child to one. Your GP practice or child’s school may also have a counsellor. Your child could also speak to someone on a helpline such as Childline, or Children First in Scotland.
Young Minds has a helpline for parents and adults worried about a child’s mental health. And our information on mental health and wellbeing has more about what counselling is and how it can help.
Encouraging your child to take their medicines
It’s important for your child to take their medicines as prescribed, to keep them well and prevent flare-ups. This can be difficult for children. Some parents have told us their children rebel, while other children may simply forget. Children who do not take their medicine are at a higher risk of flare-ups and severe disease. Parents can play an important part in helping their child take their medicines. Some of the following ideas may help:
- Make it part of their routine, just like brushing their teeth or having a bath.
- Try setting reminders on a phone.
- If your child’s medicine tastes bad, have a drink or small treat ready to take the taste away.
- For younger children, you could use a reward chart.
- Play can often be a good way to get young children to take medicines.
- Involve older children in managing their own condition. If they’re taking lots of different medicines, a medicine box with the days of the week can be a helpful way to keep track.
- Encourage older children to keep a diary of side effects, ask questions at check-ups, and take part in decisions about their treatment.
- Try to stay positive and encouraging. Remind your child that the medicines should help them to feel better, and to stay feeling better.
- Talk to your child to understand what they dislike about their medicines. They might have side effects, struggle to swallow their tablets, or simply find it a chore. Your child’s IBD team are there to help. If they know what your child is struggling with, they can give you extra support.
Try to remind your child why it is important for them to take their medicine.
Resources for children and young people
There are lots of resources and services that may be helpful for children living with Crohn’s or Colitis.
Meet our Crohn’s and Colitis cats
A colourful story book and animation to help explain Crohn’s and Colitis to children. You can watch the animation or download the book on our website.
All about Crohn’s and Colitis
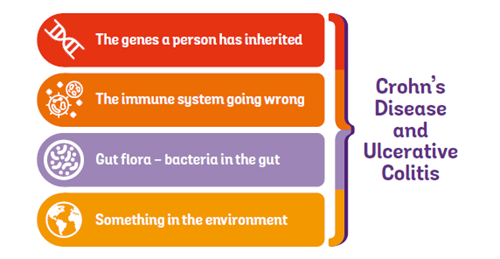
This has basic information about Crohn's or Colitis for anyone who is new to the condition. The easy-to-read format makes this a useful resource for teenagers and young people.
‘What are Crohn’s and Colitis?’ animation
A two minute animation explaining the basics of Crohn’s and Colitis.
Talking Toolkit
Your child can create their own Talking Toolkit to help them find the words to talk about Crohn’s or Colitis to their teachers and friends.
‘Telling my friends’ animation
An animation based on research with young people with Crohn’s or Colitis, funded by Crohn’s & Colitis UK.
Young person films
Five young people discuss challenges such as school, university and relationships, and share their own ways of coping.
Transition: moving to adult care
A guide for older children moving to adult care, written with the help of other young people.
Concessionary Membership
16 to 18 year olds are eligible for concessionary Crohn’s & Colitis UK membership. This means membership is cheaper or free, depending on your situation.
CICRA
CICRA are a charity that support children with Crohn’s or Colitis to live as normal a life as possible. Their website has information and videos for children and young people.
Over The Wall family camps
Over The Wall offer free weekend activity camps for children and young people with health conditions and their families. They even offer camps for siblings.